Breast Augmentation Healing Process
AFTER SURGERY CONCERNS
After you go through surgery and begin your recovery, some patients may encounter unexpected delays in the healing process. Most often these delays will not alter your final results, but do require additional instructions. This checklist will discuss the possible issues that may occur and what further treatment is recommended.
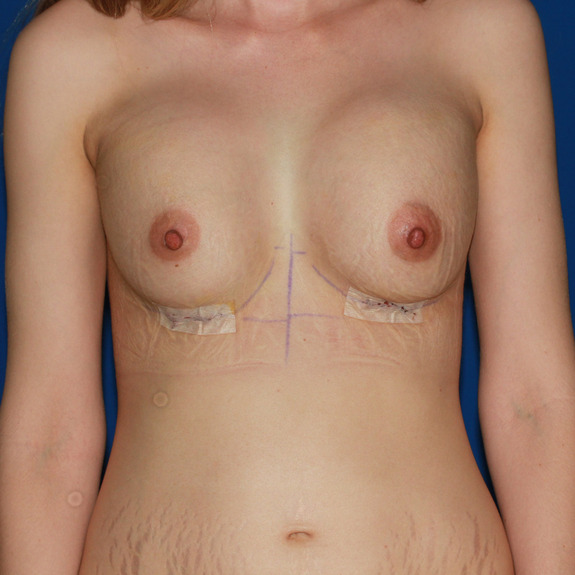
Implants appear high and nipple position low

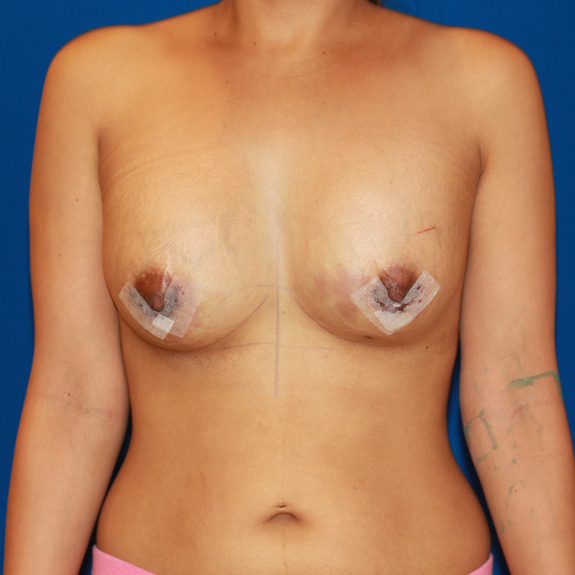
1 day post op- Implants are high and have a square appearance. Notice the nipples appear to be pointing downward.

5 months post op- Implants have dropped and popped. The breast have rounded and the nipple position has centered.
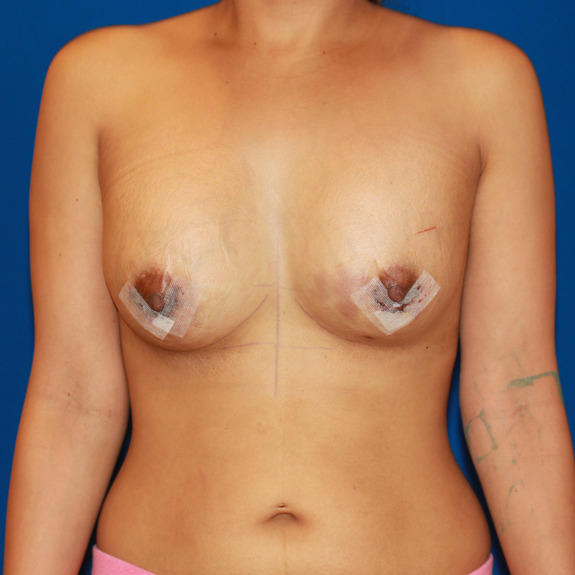
Implants appear small and high on chest
After surgery, the patient did not have any cleavage or bottom breast rounding. Implants were high and tight on chest wall.
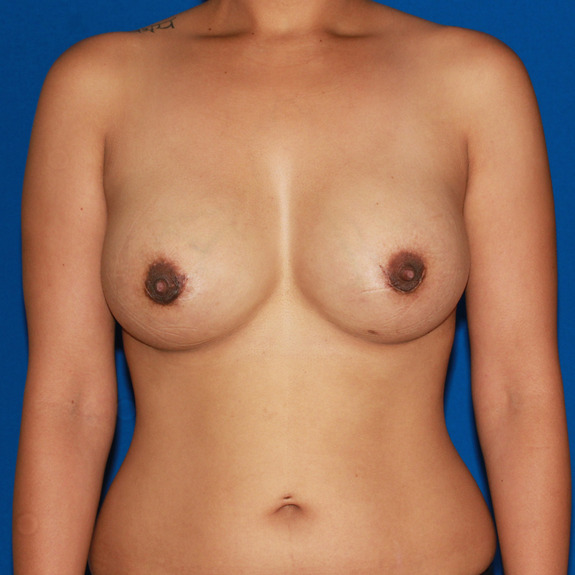
At 2 month post op, the muscles have relaxed and breast appear fuller. Patient has great cleavage and nipple position has centered.
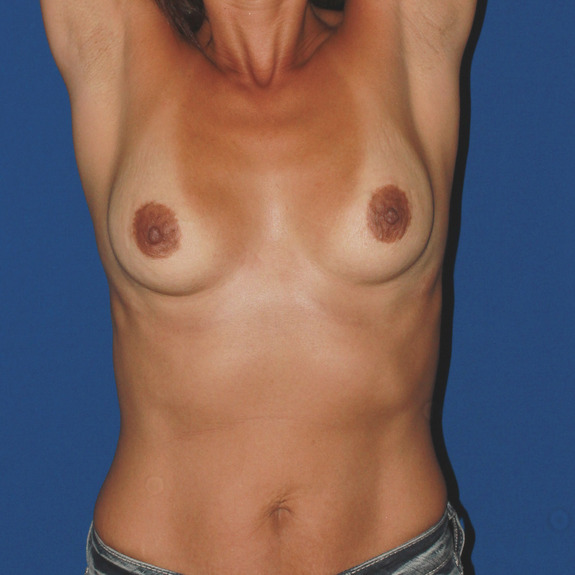
Implants appear small and high on chest
This photo was taken one day after surgery. Notice the right side slightly higher than the left. Patient has no side breast rounding.

At 4 month visit, breast have dropped and rounded out.
Implants appear small and high on chest

1 day post op- implants are high and distorted in shape. The patient is slightly hunched over due to chest tightness.

4 months post op- breast have dropped and rounded out. Patients posture has also improved.
Implants appear high and nipple position low

1 week post op- The implants are high and nipples appear low.

2 months post op- Implants have settles and nipple position has centered.
Implants appear high and nipple position low

1 day post op- Implants appear high and tight. The position of the nipples is low and facing downward.

5 months post op- Implants have dropped and taken a more natural shape. Notice the nipple position has centered.
Implants appear high and nipple position low

1 day post op- Implants are high and have a square appearance. Notice the nipples appear to be pointing downward.

5 months post op- Implants have dropped and popped. The breast have rounded and the nipple position has centered.
Implants appear small and high on chest
After surgery, the patient did not have any cleavage or bottom breast rounding. Implants were high and tight on chest wall.

At 2 month post op, the muscles have relaxed and breast appear fuller. Patient has great cleavage and nipple position has centered.
Causes
The implants are placed under the muscles of the chest wall. The muscles are normally attached to the 6th rib. However, order to allow the implants to drop this attachment is released. This allows the muscle to slowly separate from the rib. The implant, then, drops into this expanding space much like a trap door opening. This process can take up to 4 months to complete. In patients with tuberous breasts it can even take longer.
Until this “trap door” opens up, the implant has no where to go but up to the collar bones. This is why it appears so high. Until the implant drops, there is a separation of the implant and the breast tissue. The implant is high on the chest and the breast tissue remains low making the breasts appear long and unusual. This separation will go away when the implant drops. Until then, the nipples will face downward and the breast tissue will hang below the implant.
The muscles are not used to something underneath them so they try to resist stretching. In fact, they are so strong that they flatten the implant. This compresses the implant upward and makes it look smaller than it is. As the muscles relax, the implant will pop outward and appear bigger. The entire process is called “Drop and Pop”.
Treatment:
Sometimes no treatment is necessary. The implants will Drop and Pop on their own. However, massage is usually necessary. Actually, the massage is more of a squeeze and hold to help open the “trap door” and push the implants down. Invariably, one implant will be higher and more tense than the other and will need more massaging. This is usually the side that was higher before the surgery. Often, the higher one will change during the post op period.
It is important to not wear a support bra during this period unless instructed otherwise. Sometimes, a bandeau is helpful to push the implants down in between massaging. Massaging varies but usually is 1 minute each breast every 2 hours while awake.
Asymmetric dropping of implants
Asymmetric dropping of implant
Symptoms
- Implants at different heights
- One implant tenser than the other
- Implants have different shape
Asymmetric dropping but symmetric final results.

8 weeks post op: Right breast has dropped but left appears high and tight

3 months post op: Both breast have dropped and appear more symmetric.
Asymmetric dropping but symmetric final results

2 weeks post op: Left breast appears larger and higher than right breast.

4 months post op: Both breast have dropped and appear more symmetric.
Asymmetric dropping but symmetric final results

8 weeks post op: Right breast has dropped but left appears high and tight

3 months post op: Both breast have dropped and appear more symmetric.
Asymmetric dropping but symmetric final results

2 weeks post op: Left breast appears larger and higher than right breast.

4 months post op: Both breast have dropped and appear more symmetric.
Causes:
Implants almost never drop at the same rate. The reason has to do with how pliable the soft tissues of the breast are in in particular how stretchy is the muscle. One side will usually be stiffer than the other. This side will take longer to Pop and Drop into postion. In addition, swelling increases stiffness. Therefore, if one side is more swollen, typically that side will take longer to drop. In the end, they will drop to similar levels assuming they were similar before surgery.
Keep in mind, natural breasts are rarely at the same level. The breast crease defines the level of the breast. The best way to determine the level of the breast crease is to extend your arms way up to the ceiling. This will elevate the breast tissue and show where the fold is.
Asymmetric breast fold
Symptoms:
- One breast appears in higher position than the other
- The breast fold will appear uneven when arms are elevated towards the sky
Asymmetric breast folds

When her arms are in a relaxed position her breast asymmetries are not so obvious.

When arms are extended, you can see her left breast fold is higher than the right.
Asymmetric breast folds

Before: this patient came to Joseph T Cruise, MD to switch from saline to silicone. Notice her left breast appears larger.

Before: When arms are extended up, you can see her left breast fold is significantly higher than the right.
Asymmetric breast folds

After: Joseph T Cruise, MD lowered her left inframammory fold to give her a more symmetric appearance.

After: The left fold has greatly improved but still remains slightly higher. The fold cannot be lowered too much without the risk of "bottoming out".
Asymmetric breast folds

This patients asymmetries are visible when her arms are in a relaxed position. Notice the left breast is higher than the right. Breast fold asymmetries can be easier detected on patients with less breast tissue. Patients with more breast tissue will hide these asymmetries until the arms are extended to show position of their breast folds.

When patients arms are extended towards the the ceiling, you can visibly see the left breast fold is higher than her right breast fold.
Asymmetric breast folds

Breast appear symmetric when arms are in a relaxed position.

When arms are extended up, you can see her left breast appears fuller and higher than the right.
Asymmetric breast folds

Breast asymmetries appear very subtle when arms in a relaxed position.

When arms are extended up, you can see her right breast fold is higher than her left,
Asymmetric breast folds

Pre existing asymmetries are visible when her arms are relaxed at her sides.

When arms are extended up, you can see her left breast fold is higher than her right.
Asymmetric breast folds

In this case, asymmetries are visible when arms are relaxed at her sides.
When arms are extended up, you can see her left breast fold is higher than her right.
Asymmetric breast folds

When her arms are in a relaxed position her breast asymmetries are not so obvious.

When arms are extended, you can see her left breast fold is higher than the right.
Asymmetric breast folds

Before: this patient came to Joseph T Cruise, MD to switch from saline to silicone. Notice her left breast appears larger.

Before: When arms are extended up, you can see her left breast fold is significantly higher than the right.
Asymmetric breast folds

After: Joseph T Cruise, MD lowered her left inframammory fold to give her a more symmetric appearance.

After: The left fold has greatly improved but still remains slightly higher. The fold cannot be lowered too much without the risk of "bottoming out".
Causes: 85% of the time the left breast is higher than the right prior to surgery. It is very rare for the inframammory folds to have perfect symmetry. This can appear more pronounced after breast augmentation surgery. Most patients do not notice pre existing asymmetries prior to surgery. Photos are taken before surgery with arms elevated to show these asymmetries since they are often not as visible when arms are in a relaxed position. See photos above.
Treatment
The key is to massage the higher side more aggressively. Do not be afraid of “breaking” the implant. It can withstand considerable force. Our office will help you with this or go to the massage videos. These videos are tremendously helpful and outline how to manage asymmetric dropping. Make sure that your bra is not supporting the higher breast, thus, preventing it from dropping.
If there is no improvement or one implant actually begins to elevate call the office as this may be capsular contracture (hardening of the breast)
Managing your cleavage
Symptoms:
- Wide cleavage
- Natural cleavage
- Close Cleavage
- Symmastia (uni-boob)
Causes: A womans natural cleavage is defined by how close her natural breast tissue is and by how close her pectoralis major muscles attach to the sternum. To create closer cleavage a surgeon has to partially detach the pectoralis major muscle off the sternum to allow the implant to slide under the muscle and positon
closer together. Detaching the muscle off the sternum has two potential problems. One is symastia (aka uni-boob) and the other is rippling from not enough soft tissue coverage. Each surgeon has their own comfort level with how much they close the cleavage gap. Many choose to not detach the muscle at all, however, this often leaves wide cleavage.
Having done thousands of breast implants, Joseph T Cruise, MD uses his experience to get as much cleavage as possible in a safe manner. This includes partially detaching the muscle safely. In addition, Joseph T Cruise, MD has a unique method of placing the implant under not only the pectoris major but also the pectoralis minor and serratus anterior. These two additional muscles are located just in front of the axilla and thus act as a book shelf. They prevent the implants from going into the arm pit AND the push they implant toward the midline to increase cleavage.
Implant placement
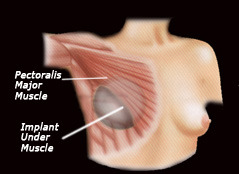
The image above show and implant placed under the pec major only.
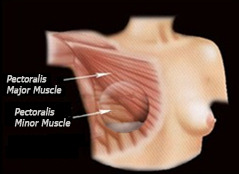
This image shows the implant placed under the pec major and pec minor muscles.
Treatment: Often, there is no need to increase cleavage as cleavage will naturally increase as the implants drop and pop. However, there is a way to increase cleavage even after the procedure. This is a very simple manuever with a bra strap convertor and breast massage. Patients often do it to achieve just a little more cleavage even if they are already happy with the result. Careful! Do not do these manuevers without consulting with Joseph T Cruise, MD as they are very effective and may in fact push the implants too close and create synmastia. The concept is to create constant inward pressure even when sleeping. This will preferentially stretch the midline skin and increase cleavage. It is most effective the earlier you begin using it. Ideally, you would begin 4-5 days after surgery and continue until you achieve your goal. It will not be effective after 6 weeks. Here is a video demonstrating the technique.
| How to creat closer cleavage | |
| Using a bra strap convertor with or without padding will push the implants closer
together if done within 6 weeks of surgery. |
|
Stitch abscess

Stitch abscess developed 6 weeks post op.

This photo was taken 2 months after stitch abscess was first noticed. The scar was not affected in final result.,
Causes: A stitch abscess is the body's reaction to a foreign object (a foreign body is any object originating outside the body) similar to a splinter. In this case, your body notices a stitch as a foreign body which can occur with both permanent and absorbable sutures. Because your body does not recognize this object it may want to get rid of it and push it towards the surface of the skin to dispose of it. This is very common in recovery and does not affect your final results. Stitch abscesses typically occur within the first 6 months after surgery.
Treatment: The best treatment for a stitch abscess is to remove the offending stitch. Come into the office and we will try to locate and remove the stitch with a sterile tweezers. Often, the stitch is almost dissolved and will go away on its own. If the abscess is draining, clean it twice a day with soap and water, put Neopsporin on it and cover it with a bandaid. Continue to tape the remainder of your incisions to take the tension off the closure. Be aware that another stitch abscess may occur elsewhere. In the end, the stitch abscess will ot affect the final result but it often causes significant redness for up to several months.
Rash healing progression

3 weeks post op: This is an example of an allergic reaction to the surgical tape. Notice how the redness is isolated to the incision where the surgical tape was in place.

7 weeks post op: This photo was taken 4 weeks after rash was first noticed. The redness has gone down and skin appears less irritated.
Causes: Many patients may develope a rash after having surgery. This typically happens in the first few weeks following their procedure. A post surgical rash can be caused by an allergic reaction to medications, adhesive surgical tape, glue, topical creams, etc.
Treatment: On rare occasions, an allergic rash may progress into a full blown anaphylaxis. This is where the throat begins to swell causing shortness of breath. This is a medical emergency and you should immediately go the the emergency room. Fortunately, this is very rare.
For the normal allergic rash, the first thing you will need to do is to assess what is the cause. This may not be so simple. If the rash and itching are around the surgical tape, the chances are it is caused by either the tape of the glue. In this case, remove the tape immediately, wash the incision with soap and water to remove the adhesive and apply hydrocortisone cream. Call the office for additional instructions.
If the rash is located over other parts of the body, it is likely you are reacting to one or more of the medications you are taking or have taken within the past two weeks. Call the office. It is likely we will instruct you to stop all medications. The important aspect to understand is that the rash will usually continue to get worse even after the offending medication has been stopped. It may continue to get worse for weeks. In addition, the skin discoloration and/or hyperpigmentaiton from the rash often lasts several months. Be patient. The discoloration typically goes away completely.
Again, call the office. Benedryl is frequently used to limit the histamine response of the rash. Topical or oral steroids may be prescribed to quickly manage the symptoms.
Wound breakdown at T junction of anchor breast lift

Wound breakdown occured 4 weeks after surgery.

Wound closed 2 weeks later.
Causes: Small wound break down is not uncommon after a breast lift. The most common location is at the T junction of an anchor lift as pictured above. Wound break down can occur if there is tension at the incision or if there is a fluid collection inside that needs to come out. It is the body's way of clearing fluid.
Treatment: If you have a wound breakdown, you will notice fluid draining. If there is tape over the breakdown, the tape will become saturated. If you see this you must remove the tape immediately. It is very important to allow this fluid to drain. Otherwise, it can pool and get infected. Therefore, if you notice any drainage under the tape take the tape off immediately and call the office. Joseph T Cruise, MD may put you on an antibiotic as a precaution. The initial drainage may have an odor to it but it should become clear and odorless. Clean with soap and water, apply Neosporin and a Bandaid twice a day until it closes.
Non-infected wound break downs routinely heal uneventfully in part because Dr. Cruies puts the implant underneath the muscles and it is typically protected. If you had a breast lift without an implant than infection is far less likely. If there is an implant it is important to keep the wound clean and covered with Neosporin to prevent the implant from getting infected. Typically, the opening will close within a couple weeks. Continue to tape the uninvolved incisions. When the wound closes tape the entire incision as normal.
Infected wounds are very uncommon but should be discussed. They are different in that they progressively become more painful and will have persistant cloudy drainage that has an odor to it. Even infected wounds are successful treated with antibiotics but it is important to recognize them immediately and call the office.
Constipation/ bloating
Symptoms:
- No bowel movement since the surgery
- Bloating
- Abdominal discomfort
Causes: Constipation is one of the most common things patients may encounter after surgery. This is particularly true if you have ANY history of constipation. We usually recommend taking stool softeners to help, but sometimes patients may require further treatment. Constipation can be caused by many aspects of surgery including anesthesia, medications, not walking as much, dehydration. Taking opiate pain medication is the biggest culprit. Such medications as Vicodin are notorious for stopping the GI tract. You need to have a bowel movement within the first few days after surgery. Those who are unable to make a bowel movement by day 3 should contact their physician for further treatment instructions. Constipation beyond this may compromise the result and can be dangerous.
Patients at high risk for constipation include:
- Anyone with a history of constipation
- Surgeries greater than 2 hours
- Tummy tucks and body lifts are particularly susceptible.
- Anyone taking opiate pain relievers such as Vicodin, Tylenol #3, etc
Treatment: Here are the steps you should take after surgery:
- Be extra prepared if you have ANY history of constipation.
- Stay hydrated
- Walk at least 5 minutes every 2 hours while awake
- Stool softeners for the first week post op
- Drink one glass of prune juice daily until off pain medications
If you do not have a bowel movement within 2-3 days after surgery stop the opiate pain medications and take plain Tylenol. The discomfort from the constipation will become much more of a problem to you than the pain of the procedure. Take an over the counter laxative such as Ex-lax or Dulcolax and call the office. If this does not work, use a Dulcolax suppository. If you do not have a bowel movement by day 5 go to Urgent Care.
Loss of sensation / numbness
Symptoms:
- Little to no sensation in surgical area
Causes: This is due to the little nerve endings, that go to the skin, either being cut or compressed during the surgery. Most patients will experience some sort of numbness after surgery. Some patients say they notice sensation coming back in as little as a few weeks after surgery. For others it can take up to several months. The length of time for sensation to come back will vary patient to patient and from procedure to procedure. Face lifts and tummy tucks take particularly long to return.
Treatment: There is no treatment for numbness. This is a common side effect from surgery and may take months and even a year to fully return.
Causes: When breast implants, or any other foreign object, are placed in the body the body forms a lining around it called a capsule. This capsule is normal. This is the body's natural response to a foreign object. In some cases this lining will continue to thicken which will cause tightening on the implant, this is know as capsular contracture. Capsular contracture is very frustrating as the exact cause is unknown, therefore, there is no specific disease process to treat.
Treatment: If symptoms are detected early on, there are steps you can take that may help soften the capsule so it is important to contact Joseph T Cruise, MD if you feel you are experiencing any of the above symptoms. Treatment consists of aggressive massage to soften the capsule. Take Vitamin E 800 units once a day. Joseph T Cruise, MD may also prescribe Singulair. Singulair is a leukotriene inhibitor which essentially decreases inflammation. This is felt to soften the inflammation within the capsule. If you follow these measures early on, we have seen an approximately 80% success rate. For the remaining 20%, Joseph T Cruise, MD recommends surgery to remove the thickened capsule and replace the implant with a textured implant. This has been quite effective but is not a guarantee that the capsule will not return. See video above.
Capsular contraction massage video
Stretch marks
Symptoms:
- Red or purple lines on the breast.
Causes: Rapid stretching of the skin from the implant causing tearing of the dermis. Stretch marks are caused by stretching of the skin at a faster pace than the skin elasticity can handle. Putting the implant under the muscle has the advantage of reducing the tension on the skin. This is because the muscle actually resists the rapid expansion of the skin. This is why the implant appears flattened and compressed immediately after surgery. The muscle is absorbing the expansion. Over time, the muscle stretches but by then it has given the skin a chance to stretch on its own.
Obviously, very large implants are more likely than smaller ones to cause stretch marks. However, for as common as breast augmentation is, stretch marks remain an uncommon long term problem.
Treatment: The best way to prevent stretch marks is to keep the dermis moistured.Coco butter or shea butter are often used for this purpose and seem to help. There is, however, no guarantee. Women with a family history of stretch marks are more likely to get them. The good news is 1) stretch marks are relatively uncommon especially if you do not go with a large implant and 2) they typically fade quite nicely if they do occur. See images below.
Stretch Marks- healing progression

Stretch marks started to appear around 2 months after breast augmentation surgery

At patients 12 month follow up, the stetch marks had faded away to nearly nothing and breast have rounded.
Throat irritation after general anesthesia
Symptoms:
- Sore throat
- Difficulty swollowing
- Visible white film in the back on tonsils and uvula
- Hard to talk after surgery
Causes: The irritation will typically be at two different levels depending on the type of tube that was put in. For example, our Anesthesiologist uses a Laryngeal Mask Airway (LMA) which is really nice because it is like a sponge that rests in the back of the throat. An LMA may cause irritation to the back of the throat i.e uvula and tonsils. The other type of tube is a Endotracheal Tube (ET tube). It goes all the way through the vocal cords and into the trachea. This tube can cause vocal cord irritation. This will make it hard to talk.
Treatment: Throat irritation is usually treated with frozen ice cream or frozen yogurt along with Chloriseptic Lozenges. The ice cream will decrease the swelling and the Chloroseptic contains phenol which numbs the mouth and throat. It is OTC. Symptoms usually start getting better in as little as 3-10 days starting treatment. See example photo below.
Throat irritation

This is an example of a throat irritation after generalanesthesia using LMA.